Do I really need to stretch my hamstrings?
April 4, 2016
Benefits of Stretching after Workouts
May 18, 2016
What is the piriformis muscle?
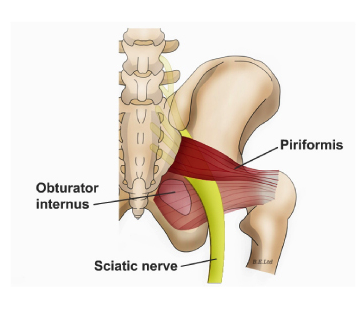
Piriformis muscle is a flat muscle located deep in the gluteal region and attaches into the femur (thigh bone). The piriformis muscle acts as a hip abductor (moving away from body) when the hip is flexed as well as external rotator when it’s extended (turning the leg and foot outwards). Piriformis muscle plays an important role in hip stability, which is essential when walking, climbing up stairs, shifting weight from one foot to another as well as hip and leg motions used in various sports.
Sciatic Nerve:
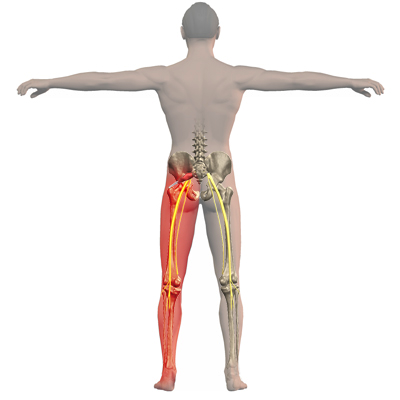
The sciatic nerve emerges from the lumbar spine (lower portion of the spine), runs underneath the piriformis muscle and extends down the thigh and leg supplying the muscles of the lower limb.
Piriformis syndrome is a condition in which the piriformis muscle compresses on the sciatic nerve causing pain in the buttocks.
Signs and Symptoms of piriformis syndrome:
- Pain in buttocks, hip. Pain may be characterized as dull ache or burning pain in buttocks.
- Pain down the back of the thigh, and leg (known as sciatica)
- Numbness/tingling in buttocks, back of the thigh and leg, and sometimes sole of foot.
- Increased pain with climbing stairs, prolonged sitting, walking.
- Limited hip mobility
Causes of Piriformis syndrome:
Piriformis syndrome is generally caused by tightness or spasm in the muscle due to overuse or injury. The following are possible causes:
- Inactive/weak gluteal muscles caused by overactive hip flexors that result from prolonged sitting. Common in people with desk jobs who sit for long hours.
- Overuse injuries resulting from activities done in sitting position such as rowing, cycling
- Muscle imbalances (such as tight hip adductors, weak hip abductors) causing the piriformis to shorten and contract; which therefore can compress on the sciatic nerve. Common in runners and cyclists.
- Stiffness or decreased mobility of sacroiliac joint, causing shearing forces on the piriformis.
- Over-pronation of the foot causes the knee to rotate inwards, forcing the piriformis to work harder to prevent over-rotation of the knee. This results in overuse of the piriformis, which becomes tight and may compress the sciatic nerve.
How is it diagnosed?
Piriformis syndrome is usually diagnosed based on patient’s history of symptoms and clinical presentation. There are some clinical tests that can be done during physical examination, which may elicit the symptoms of piriformis syndrome. This includes the FAIR test (Flexion, adduction, Internal rotation), testing piriformis muscle or stretching it, which may irritate it and/or provoke the sciatic nerve. However tests should be done to rule out Disc Herniation or spinal stenosis.
Prevention:
Piriformis Syndrome that is not due to trauma but rather secondary causes such as prolonged sitting especially on hard surfaces, physical activity, poor training mechanics.. etc can be prevented.
Prevention strategies include:
- Avoid sitting for too long at your desk.
- Use padded cushions on hard surfaces
- Warm up well before training
- Daily stretching routines
- Strengthening exercises (especially core muscles, glutes, hip abductors)
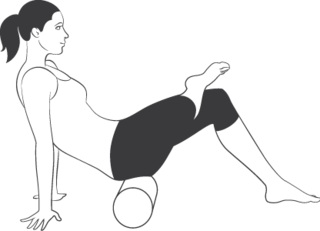
- Foam rolling
- Good sitting posture and office ergonomics
Treatment:
Conservative treatment is usually done through physiotherapy or chiropractic treatments which such as:
- Myofascial release or deep tissue massage
- Dry needling with or without electrical stimulation
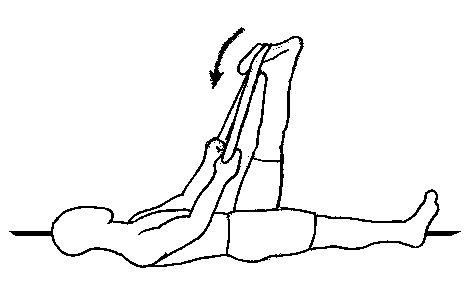
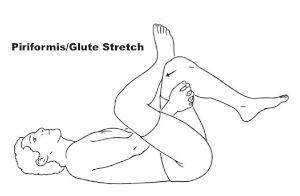
- Stretching exercises for piriformis, hip flexors, hamstrings
- Strengthening exercises for hip abductors, hip extensors, core muscles.
- Hip joint mobilization
- Nerve stretching exercises.
- Ice packs or cold packs.
Piriformis syndrome has very good prognosis and conservative treatment through physiotherapy and rehabilitation programs have shown to be very effective resolving the symptoms.
Nermine.